Healthy People Healthy Trails program aims to get people healthy while connecting them with nature
BY ZAC EZZONE
Through a growing program in Santa Barbara County, participating doctors are prescribing some patients to take a hike.

The effort started in 2015 after Mark Wilkinson learned about Healthy Parks Healthy People, a program within the National Parks Service that promotes the link between human health and time spent in nature.
On its website, the parks service points to research and evidence supporting the notion that more time spent in parks leads to better health. This includes research published in Scientific Reports—a Nature Research journal—last year that suggests spending at least two hours in nature each week is associated with good health.
Wilkinson, who is the executive director of the Santa Barbara County Trails Council, said he knew the county needed its own version of Healthy Parks Healthy People to introduce people who are unfamiliar with nature to the trails and other outdoor opportunities available locally.
“This is the kind of thing we need in the county to get people to appreciate the great natural resources we have … but bring in the health component that’s so critical,” Wilkinson said.
To get started, Wilkinson first secured assistance through the National Parks Service’s Rivers, Trails, and Conservation Assistance Program, which assigns staffers, such as Patrick Johnston, to assist nonprofits, schools, public health departments, and other community groups with projects.

Johnston said after a year of working with the trails council and various health care groups—such as Sansum Clinic and CenCal Health—throughout the county, Healthy People Healthy Trails launched in 2016. At its inception, the program centered on South County, but has since expanded into Lompoc.
Members involved with the program work in various ways to encourage people to get walking outside, but the program centers on establishing connections with doctors who prescribe patients to take walks or hikes as part of their health care regimen. If a doctor administers this prescription, the patient is given either physical or electronic copies of trail maps and other material Healthy People Healthy Trails creates, Johnston said.
The map includes technical aspects of the trail such as its distance, surface material, and elevation changes, as well as a description of the area and amenities available there. Although this is the first time he’s worked on a project like this, Johnston said there’s been an effort nationwide to implement prescription trail programs.
“It wasn’t about telling a patient to go out,” Johnston said. “It was about here are some concrete options to take a walk and here’s something you can see and do on that walk.”

So far, Healthy People Healthy Trails has been able to establish relationships with Sansum Clinic as well as the county Public Health Department. Wilkinson said doctors with Sansum Clinic gave 400 prescriptions last year—but he noted that the program doesn’t have a way for tracking what the patients do with these prescriptions.
Emily Casarez, director of community health with the Healthy Lompoc Coalition, said the organization got involved with Healthy People Healthy Trails in late 2018, which helped expand the program into Lompoc. She said a few doctors at the Lompoc Health Care Center—which is part of the county Public Health Department—are working with the group and giving out trail prescriptions; she’s hoping to grow this number in 2020.
Healthy People Healthy Trails has created a few maps for trails in Lompoc, including one for a roughly 2-mile loop trail at the Burton Mesa Ecological Reserve as well as one for a roughly 3-mile loop trail at La Purisima Mission State Historic Park. These maps are available on Healthy People Healthy Trails’ website.
Wilkinson said he plans to create additional maps for places where Healthy People Healthy Trails already has a presence, but he would also like to see the program expand farther north into Santa Maria. Another opportunity he’s hoping to address is how the program establishes connections with independent doctors throughout the county.
“We would hope that by the end of the year we can be referred to as a countywide program because everything came together,” Wilkinson said. “That might not all come together this year, but we’re in it for the long haul.”
Reach Staff Writer Zac Ezzone at [email protected].
The direct primary care model revitalizes the doctor-patient relationship
BY KAREN GARCIA
PJ Lloyd has a unique living situation due to her career in digital marketing, technology marketing, and web development. She spends half her time in Minneapolis and the remainder of it in California.
Her primary care doctor, who Lloyd has seen for several years, is in Minneapolis, but Lloyd said her overall experience hasn’t been positive.
She’s recently experienced a health issue that she’s tried to communicate to her doctor but found it challenging.
“It was as though he wasn’t listening to the symptoms and the issues I was having. It was more of a quick in-and-out,” Lloyd said.

Lloyd explained her situation to a friend on the Central Coast who referred her to Dr. Lindsey Faucette, who handles her practice a little differently than the chain hospitals and concierge medical practices in the area.
Dr. Faucette follows the direct primary care model, which isn’t new but is becoming more prevalent throughout the U.S.
As opposed to hospital chains—nonprofit and for-profit—that bill insurance companies for their patients, direct primary care cuts out the middleman by taking direct payment from the patient through a flat monthly rate. The model decreases the cost of seeing a doctor and increases the amount of time a doctor can spend with a patient.
Dr. Faucette opened her practice, the SLO Health Center, in San Luis Obispo in 2019.
Lloyd hasn’t seen Dr. Faucette in person yet, but she’s sent the doctor her medical records, and they’ve had several phone calls—the initial consultation and conversations about Lloyd’s overall health as well as her recent concerns.
“[Dr. Faucette] made me feel like my situation, at that point she was on the phone with me, was the most important part of her day,” Lloyd said.
***
Sitting in her practice room with plenty of natural lighting, Dr. Faucette told the Sun she could remember the exact moment she realized she didn’t want to be in a modern hospital setting.
During residency training in New York City, where she trained in a federally qualified health center on Union Square, she was dissatisfied with the structure of the clinic because she rarely saw patients she knew.
“It was more often whoever just wound up on my schedule, and that tends to happen when these [hospital] systems get too big,” she said.
Dr. Faucette said she remembers being in her program director’s office and asking for more continuity with patients.
“We have to be able to see our patients and see what happens to them over time,” she remembered telling her program director.
Dr. Faucette moved on to being a practicing physician at a hospital in California with the same issues: No doctor and patient foundation, the call center for the hospital was outsourced, and there wasn’t enough time to understand each patient’s needs.
The modern hospital setting didn’t make sense to Dr. Faucette, whose medical background is focused on osteopathic and family medicine. Osteopathic medicine has all the benefits of modern medicine but it emphasizes health promotion and disease prevention by taking an overall wellness approach. She believes that part of that approach is taking the time to get to know the patient and understand their medical history.
For seven years, she was a physician and educator at a family medicine residency. Dr. Faucette decided to leave after learning about the direct primary care model and the Direct Primary Care Alliance, a membership organization for direct primary care physicians who partner with their patients to provide primary care services under a flat periodic membership fee.
In 2019, Dr. Faucette left what she calls “corporate medicine,” following her lifelong dream of forming relationships built on trust with her patients. The SLO Health Center is subscription-based—patients pay a flat monthly rate based on their age. Through her practice, Dr. Faucette offers no co-pays, an unlimited number of visits, accessibility to her through email, text, or phone, as well as home visits. She’s also able to call or text doctors and laboratory offices on her own time, to talk about her patients or get laboratory results.
For a new patient, Dr. Faucette schedules a two-hour appointment to understand the patient’s history, his or her concerns, and come up with a unique comprehensive plan. Follow-up appointments can range from 15 to 30 minutes, depending on the situation.
She said she’s able to offer these benefits because she’s keeping her patient list to 200 to 300 patients—as opposed to the typical 1,000 to 3,000 patients per doctor. The increased time for health care delivery comes from the doctor not having to bill insurance, write down the codes for every check and procedure done, or submit medical notes to an insurance agency.
***
Physician Dr. Julie Gunther from Boise, Idaho, was the first to open a direct care practice in Southwest Idaho in early 2014. She’s also one of the founding members and current president of the Direct Primary Care Alliance—the physician run, founded, and direct primary care physician organization.
Dr. Gunther said the heart of the organization is to revitalize direct medical care to patients, but it came about because of physician suicide and burnout.
According to a review of 10 years of literature presented at the American Psychiatry Association in 2018, an estimated 300 to 400 doctors kill themselves each year.
A recent online survey of doctors completed by the American Medical Association found an overall physician burnout rate of 44 percent, with 15 percent saying they experienced colloquial or clinical forms of depression. Physician burnout, according to the Agency for Healthcare Research and Quality, is a long-term stress reaction marked by emotional exhaustion, depersonalization, and a lack of sense of personal accomplishment.
Dr. Gunther was one of many physicians who experienced burnout and said direct primary care saved her and gave her the ability to be the doctor she set out to be.
On top of this resurgence of direct medical care, Dr. Gunther said physicians are going back to being the “Swiss Army knives of medicine”—doctors who are trained and can treat the entire body (in most cases).
“Family physicians are sort of reclaiming their scope of practice and saying, ‘You know I can take that off a patient’s back and it costs me 10 bucks in supplies and a half hour’s time,’” she said.
It significantly reduces the amount of money a patient spends, she said. An example would be trying to get a referral to a dermatologist, where patients pay for the initial consultation with the specialist plus the cost of the procedure.
However, Dr. Gunther said that the direct care isn’t the same as concierge medicine. Both are alternative ways to deliver health care that have shifted from the modern business model, but she said the end goal and spirit of each model is different. While concierge physicians can provide complete care for a reasonable fee, these practices typically take insurance and charge a fee on top of that.
In a typical direct primary care practice, it’s just a flat rate, Dr. Gunther said, which is normally less than $100 per person per month. It doesn’t matter whether the patient doesn’t have an insurance card, a green card, or a Social Security card—that person will be provided medical care.
***
Appalenia Udell, a Colorado-based health lawyer for doctors, helped write the Colorado Direct Primary Care Act of 2017, which exempts practices following the model from state insurance regulations.
Udell is now working on making Medicare accessible for direct primary care physicians. She issued a letter of intent to the Centers for Medicaid and Medicare Services—a division of the U.S. Department of Health and Human Services that administers the Medicare program—in December 2019 saying that she wants Medicare to be a direct contracting entity.
“We just want to work with direct primary care practices and enable them to get their monthly fee through Medicare, rather than not seeing Medicare beneficiaries at all, or going through a traditional fee for service,” she said.
She wants direct care practices to be able to partner with state-based Medicare programs, including Medi-Cal. Patients using Medicare tend to have complex or chronic health conditions, Udell said, that have been shown to benefit greatly from enhanced care offered by the direct primary care model, while simultaneously addressing the heightened cost of care for these patients.
The process to approve the initiative includes submitting a formal application (along with a list of physicians who are behind the initiative) by Feb. 25 and implementing the initiative by June 30. If successful, the initiative would be available Jan. 1, 2021.
Udell joined Dr. Faucette in bringing the idea to SLO Mayor Heidi Harmon. Harmon told the Sun she thinks the model could provide a level of care that would really benefit all kinds of people in the community.
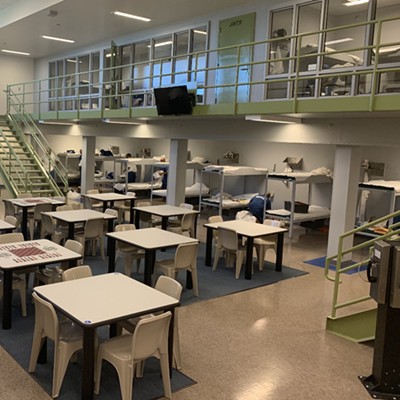
Aside from providing an alternative method of affordable health care delivery to city employees, the community at large, and Cal Poly students, the direct care model could also benefit homeless individuals who are on Medi-Cal or Medicare. SLO County Jail inmates could receive this care while in custody, and transgender youth and young adults could receive direct gender affirmation care.
“Until we make something like single-payer health care a reality in our country, these other models are providing deeper understanding and approach to medical care,” Harmon said. “I’ve tried to create a community of care here in SLO, and the type of medical care [Dr. Faucette and Udell] are talking about really adds to that.”
New Times Staff Writer Karen Garcia can be reached at [email protected].
In recent years, the medical community has taken Reiki more seriously
BY WILLIAM D’URSO
Andreea Saileanu-Martin’s journey into alternative medicine began nearly two decades ago after she suffered a miscarriage. Looking for relief, a friend of hers suggested Reiki. The practice helped her move away from the dampening energy of her grief. It was a new type of healing for Saileanu-Martin.

“I instantly felt more grounded,” the 39-year-old said. “It was really interesting to me because it was not massage but did some of the same things.”
Reiki practitioners and recipients say it can offer stress relief and muscle relaxation. The discipline seeks to manipulate or redirect the energy within a person to boost healing, increase calmness, or tamp inflammation.
The Japanese practice starts with a hovering of the hands, just a few inches from the body. Perhaps over a shoulder, a head, even a person’s unmentionables. Those hands can stay put or move, helping push stagnant energy back into a body’s natural flow.
“If you have a trauma or something else going on in you, that energy stagnates,” she said. “Reiki releases that stagnation.”
To the uninitiated, it appears to be merely a system of healing with little support from clinical research and only a loose credentialing for those who practice it.
Saileanu-Martin, who runs Wholeistic Fruition Wellness out of Santa Maria, spent her early professional years learning massage therapy, especially the deep-tissue techniques of the long-held tradition of Swedish massage. But the physical nature of that discipline caught up to her. She said massage therapists tend to even out their workload throughout the week and avoid busy schedules of 30 or more hours—seeking to avoid injury and save their bodies so they can help heal others.
“We’re energetic beings,” she said. “We all have energy.”
Although she refers to it as energy, others refer to it as the electrically charged nervous system, which runs throughout the human body and affects all manner of functions.
Eventually, Saileanu-Martin sustained her own malady, a shoulder ailment doctors told her would need surgery. Instead, she tried other forms of healing, including Reiki, and she said that she hasn’t had to resort to invasive forms of surgery.
But Saileanu-Martin stresses that Western medicine is vital and has many crucial components. Reiki and other types of healing are simply meant to offer a deeper range of options when the conventional, mainstream practices falter.
Reiki practitioners often go through three stages of training, although California doesn’t have a formal process of accreditation.
The first level prepares people to self-heal through Reiki, the second offers preparation to administer Reiki on others, and in the third—Reiki master—practitioners teach the discipline to other students.
Techniques can vary. Saileanu-Martin said a common phrase for one of the techniques in the profession is “lay hands.” While many practitioners don’t actually put their hands on clients, Saileanu-Martin does, recalling her days in massage and her other discipline of neural palpation. In that practice, she lightly probes the nervous system, helping along the little currents of energy the body is known to produce.
The costs of Reiki also vary. Saileanu-Martin sells her services for $1 a minute, slightly more than the costs for some of her other offerings. Other practitioners tend to charge much more, with $125 being a common rate in Los Angeles, according to Yelp.
Reiki has long had a dubious reputation: a healing art of ancient origins once considered the domain of hippies, swamis, or, more simply, the very strange.
But some hospitals nationwide have increased attention to the art, and UCLA has conducted research on Reiki, according to the school website. The service, while it does require special training, isn’t miracle work.
“I don’t think I’m any kind of magical unicorn,” Saileanu-Martin said. “It’s not just a bunch of woo-woo standing naked in a field burning sage. There’s merit behind it.”
Theories behind how Reiki actually works differ. Saileanu-Martin said there are some who say it’s spiritual—religious, even. Others think it’s just another way for the body’s natural powers of healing to be redirected to problem areas.
Either way, Saileanu-Martin says what’s the harm in it? Reiki is a discipline designed to help people relax and heal. Even if it doesn’t accomplish the intended healing, she says it doesn’t hurt to try.
Saileanu-Martin is not your typical health care professional—she no longer has an office, although she once had a space in Orcutt. Now, she offers a mobile service, catering to many clients who aren’t particularly mobile on their own.
Next, she wants to get into dentist offices, snap on some white gloves, and gently probe people’s mouths, bringing her healing techniques to locals’ oral health.
“Putting Reiki into practice, it’s everything,” she said.
Contact Staff Writer William D’Urso at [email protected].